DISCLAIMER: Mito Red Light devices are not clinically proven to diagnose, treat, cure, or prevent any medical conditions. Mito Red Light devices are low / risk general wellness devices aimed at affecting the body through supporting cellular function. The scientific studies referenced in this article are for educational and informational purposes only and are meant to educate the reader on the exciting and growing field of phototherapy. To see a list of precautionary warnings and contraindications, click here
Medically Reviewed by | Heidi Wright, BSN, RN, PCCN
Table of Contents
- What is Sleep?
- Sleep Cycles
- Circadian Rhythm
- Health Impacts of Inadequate Sleep
- Sleep-Related Disorders
- Sleep Hygiene
- Red Light Therapy and Sleep
- Improvement in Underlying Factors
- Using Red Light Therapy For Sleep
- Mito Red Light
- References
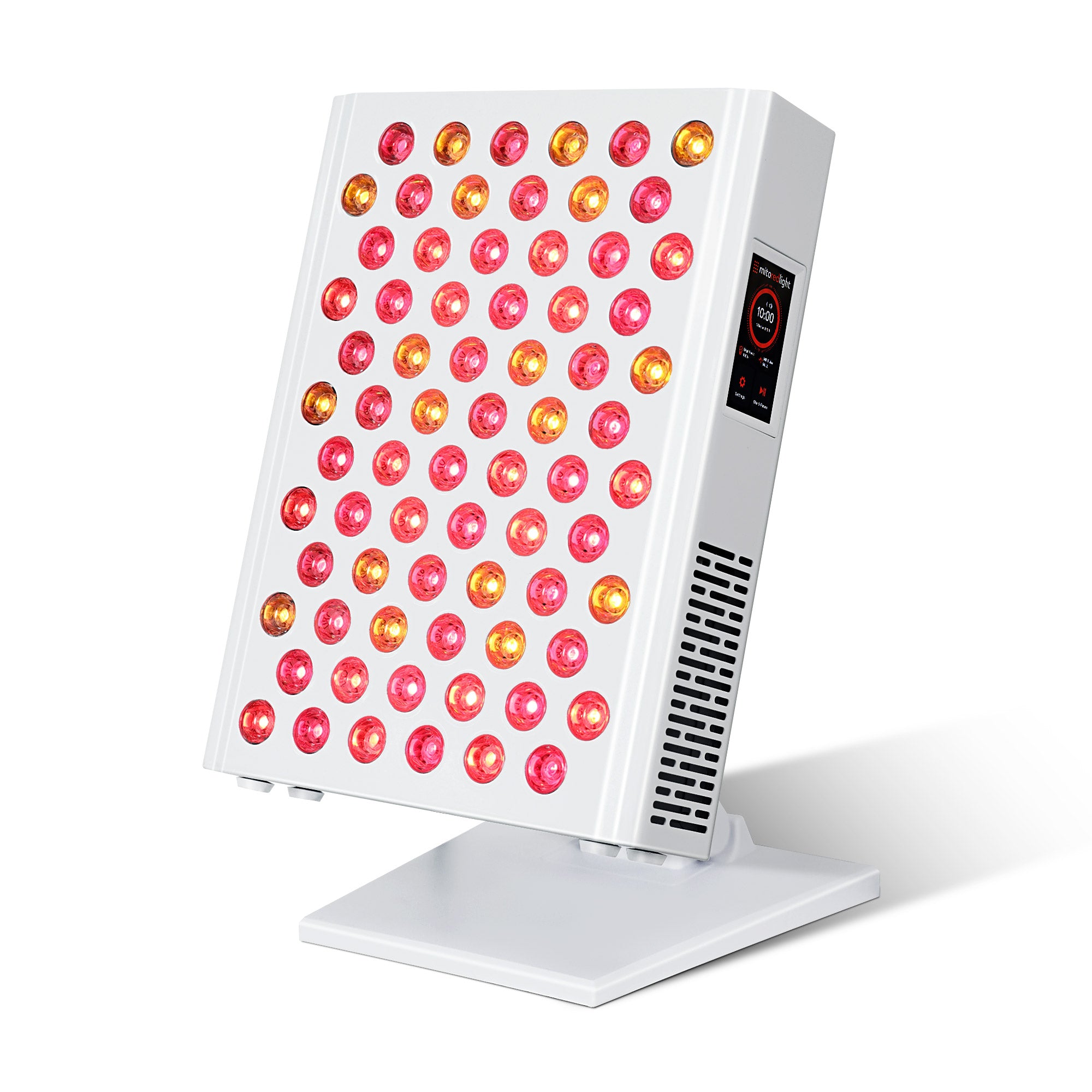
One of the most common desired red light therapy benefit is the hope that regular use will improve the quality of their sleep. Red light therapy uses both red and infrared wavelengths of light that are irradiated on the body. This form of therapy was discovered by NASA [1] researchers in the mid-1990s and has become popular due to its ease of use, safety, and the effects that people experience while using it.
People use red light therapy for a variety of sleep issues, from improving the quality of their skin to speeding wound healing. Red light therapy is thought to work by stimulating mitochondria [2], small subcellular organs in your cells that produce energy and help to reduce inflammation. This effect explains many of the beneficial effects of red light therapy that people using it report experiencing.
While red light therapy has been used for applications like wound healing for almost three decades, using it for sleep is a newer application. The use of red light therapy for sleep emerged as a potential application in 2012 when a study involving a group of athletes found sleep-related benefits. Since then, research into the benefits of red light therapy for sleep has continued to expand.
What is Sleep?
To understand how red light therapy benefits sleep [3], it is first necessary to understand what sleep is and how it works. When you stop and think about it, the idea of sleep can seem quite strange. We sleep every day, spending about one-third to one-fourth of our lives in a semi-conscious state, unaware of most changes in our surroundings.
During sleep, we enter an altered state of consciousness, with most of our sensory functions inhibited. Most muscle activity is suppressed, and almost all voluntary muscles are completely inhibited, creating a form of paralysis that only lasts during sleep. During sleep, the mental imagery called dreams occurs. These often take the form of a story, often with an unusual narrative, and can appear real at the time.
There is still much about sleep that is not fully understood, but medical researchers do know that sleep is essential to good physical, cognitive, and emotional health. Sleep deprivation can lead to many negative health consequences, and getting less than the recommended 7-9 hours of sleep each night can lead to health problems over time.
Sleep Cycles
One of the core sleep-related concepts is sleep cycles. During sleep, your brain has rhythmic brain waves that take on different forms depending on what stage of sleep you are in. Changes between the stages of sleep are detectable by monitoring brain waves. For sleep to be fully restorative, you need to go through several of these cycles. Each cycle lasts about 90 minutes.
The stages of sleep are progressive, starting at stage one and progressing to stage four, then progressing back to stage one. The stages of sleep [4] are:
- Stage One - Stage one sleep is the lightest stage of sleep and is the type of sleep you are in when you doze. In this stage, you are very easy to wake up; however, you will normally quickly progress to the next stage of sleep.
- Stage Two - During stage two sleep, the body begins to slow normal functions like breathing and heart rate. The body’s temperature begins to drop and it becomes more difficult to be woken up by your surroundings. A person will spend about half of their time asleep in stage two sleep during a normal night.
- Stage Three - Stage three sleep is also known as deep sleep or slow-wave sleep. During this stage, it becomes more difficult to be awakened. Breathing, heart rate, and temperature are all decreased during this stage. Stage three sleep is very restorative and occurs mainly in the first half of the night.
- Stage Four - Also called rapid eye movement (REM) sleep, stage four sleep is different from other stages. The brain becomes very active during REM sleep. At the same time, all muscles in the body become paralyzed except for breathing muscles and eye muscles. The eyes move rapidly during REM sleep, giving it its name. Most dreams will normally occur during REM sleep, although dreaming can occur at any time while asleep. REM sleep is considered to be essential to many important cognitive functions.
Disruptions in sleep can interrupt sleep cycles, making the sleep you are getting less restorative. People who wake up frequently while sleeping may not experience much or any stage three and stage four sleep, making them feel tired and causing negative effects.
Circadian Rhythm
Another important sleep-related concept is the circadian rhythm [5]. This biological rhythm operates as the body’s internal clock, and affects many different processes in the body, impacting emotions, hormones, protein, production, and much more. However, the clearest example of the circadian rhythm is the sleep-wake cycle.
There are many different factors that can impact your biological clock, but light affects it most. Light entering your eyes not only creates an image of the world around you, but it also subconsciously affects your circadian rhythm, telling you when it is time to be awake and time to go to sleep.
As light wanes during the day, the body begins to produce a hormone called melatonin. Melatonin [6] plays an important role in promoting sleep, transitioning the sleep-wake cycle into the sleep phase.
While the reduced intensity of light is important to stimulating melatonin release in the evenings, the type of light is also very important. High-energy blue shades of light (emitted from LED light bulbs, televisions, smartphones, and other devices) suppress melatonin production, while orange and red wavelengths do not have the same effect. Recognition of how blue light at night affects sleep patterns has led many electronic manufacturers to install nighttime settings that reduce blue light in laptops, phone screens, and televisions, and use warmer shades that have less effect on the circadian rhythm. Not sure if your device offers a night light option? Check with the manufacturer or look under the “settings” portion of your device.
Health Impacts of Inadequate Sleep
Failing to get enough sleep or the right kind of sleep can have many negative effects on your health. The health conditions that inadequate sleep causes can lead to decreased life span [7] in addition to the negative effects experienced on your day-to-day quality of life.
Hypertension
A lack of high-quality sleep can cause hypertension [8] or elevated blood pressure. Blood pressure increases after a night of insufficient sleep, and prolonged sleep problems can lead to chronic hypertension. This increases your risk of heart disease, stroke, and heart attack.
Memory Issues
Sleep plays an important role in consolidating memories and helping new memories to form. Sleep deprivation can lead to short-term and long-term memory problems that can make tasks like learning or functioning at work more difficult.
Mood Changes
Sleep has a role in reducing stress and improving mental well-being. When someone is partially or fully sleep-deprived, it can cause mood changes. This can lead to irritability, anxiety, depression, or other mood problems that will not resolve until adequate sleep occurs.
Weakened Immune Response
During sleep, certain components of the immune system become more active. While there is still research into exactly how sleep and the immune system are related, medical scientists know that lacking sleep, even over a short-term basis, can lead to a suppressed or weakened immune system. This can make you more susceptible to infections and other illnesses.
Problems Thinking and Concentrating
Inadequate sleep can affect memory but can also affect the ability to think and concentrate. While researchers do not fully understand how sleep affects the brain, medical science does tell us that sleep affects how well the brain is able to function, improving how well we can concentrate and function cognitively throughout the day.
Weight Gain

Poor sleep increases your appetite and makes you less active throughout the day because you feel more tired. This leads to increased caloric intake while reducing the amount of energy that you burn. These effects cause increased weight gain. Studies show [9]. that the amount of sleep you get directly correlates with having a better, healthier weight.
Risk of Diabetes
Not getting enough good sleep increases your risk of developing diabetes. Increased weight gain does play a factor; however, inadequate sleep also reduces how sensitive your cells are to insulin. As insulin sensitivity decreases, your body is less able to regulate blood sugar levels and is more likely to develop diabetes. If you have type 2 diabetes, getting adequate sleep has been shown to improve your blood sugar levels [10].
Accidents
Because a lack of sleep can impair cognitive function, inadequate sleep can lead to an increased risk of accidents. In some states, it is illegal to drive when you have been without sleep for more than 24 hours because of this risk. Operating heavy machinery, swimming, or driving are all situations where the risk of accidents may increase when you have not had adequate sleep.
Sleep-Related Disorders
Many times people do not get enough sleep simply because they do not take the time to get the sleep that they need. Setting aside 7-9 hours to sleep may not happen for some people. In some situations, however, people may find that even though they set aside enough time, they do not get the rest they need.
Sleep disorders affecting how restorative your sleep is often involve one of two key problems:
- An inability to get to sleep
- Difficulty staying asleep
There are also sleep-related disorders that do not affect how much sleep you get but are still sleep-related.
Difficulty sleeping is becoming a more prevalent problem, with rates of insomnia increasing in many countries. One factor that may be affecting sleep is decreased exposure to near-infrared light from sunlight. Increased time indoors and new window technologies that filter out infrared light have decreased humans’ exposure to sunlight. It is hypothesized that infrared exposure during the day increases melatonin levels, helping to promote high-quality sleep at night.
Additionally, increased exposure to blue light at night, which is known to suppress melatonin production, is becoming more and more prevalent at nighttime screen exposure becomes more common. Changes in exposure to different forms of light may play a role in the increased incidence of sleep-related disorders.
Insomnia

Insomnia is a very common sleep disorder and is a medical term used to describe difficulty falling asleep or staying asleep, especially when this difficulty sleeping affects your life while you are awake. Insomnia can be a short-term problem or can be chronic, affecting you for more than six months. While any insomnia is frustrating, chronic insomnia can be particularly impactful on someone's life.
Insomnia may occur for no discernible reason but is commonly related to an identifiable cause. Some of the common causes of insomnia include having an increased level of stress, having a mental health disorder, hormonal fluctuations, abnormal sleep schedule, and many other potential causes.
According to the Sleep Foundation, risk factors for insomnia [11] include:
- Female sex
- Age
- Socioeconomic status
- History of being a light sleeper
- History of difficulty sleeping while stressed
- Recent stress in life
- Tendency to be preoccupied with your health
- Mood disorders
- Certain medical problems
- Heavy alcohol use
- Heavy caffeine use
- Domestic abuse
- Disrupted home environment
- Having a blood relative with insomnia
- Lack of consistent sleep schedule
Insomnia can be treated with some medications, education, or certain types of therapy. While medications can help, they may also include undesirable side effects or may lead to a situation where using the medicine is necessary to sleep. While non-pharmacological treatments are typically preferred, some people may require medicines. Someone with insomnia should speak with their doctor about what types of treatment will be best for them.
@mitoredlightofficial Feeling grumpy and restless? 😡 Red Light Therapy can improve your sleep, making you feel more restored after a good night of snoozing. 😴 Learn more about how RLT can make you sleep deeper: link in bio! #MitoRedLight #RedLightTherapy #SleepRoutine #SleepTok #SleepHack ♬ Hey It's Me - Official Sound Studio
Obstructive Sleep Apnea

Obstructive sleep apnea is a common sleep-related problem; however, many people with this condition may not be aware that they have it. Many of the signs of obstructive sleep apnea are not obviously related to the condition, and someone who has it is unlikely to recognize the signs of this condition, especially if they sleep alone.
Obstructive sleep apnea occurs when the airway becomes obstructed during sleep. This typically occurs because the tongue relaxes, falling to the back of the throat. This occludes the airway, making it impossible to breathe. This leads to a period of being unable to breathe called apnea. After several seconds of apnea, the body will awaken the person sleeping just enough for them to move their tongue out of the way of their airway and resume breathing again.
The entire process of a period of apnea during sleep due to obstructive sleep apnea will wake up the person who is sleeping, but not enough that they will consciously be aware that they actually woke up. Periods of apnea can occur dozens of times during the night, making it impossible to reach any stage of sleep beyond stage one and stage two sleep. This can result in the person with obstructive sleep apnea sleeping for a full eight or nine hours but having never experienced full, restorative sleep.
Someone with obstructive sleep apnea will feel tired throughout the day, ready to fall asleep at a moment’s notice. People with obstructive sleep apnea will typically be “snorers,” and the person they sleep with will often report that they snore loudly, have periods where they stop breathing, or that they make choking noises in their sleep.
Someone who has very frequent episodes of obstructive sleep apnea may sometimes actually wake up more fully during an episode and be aware that they sometimes stop breathing during their sleep. If this is the case, the episodes that they are aware of are often just a tiny fraction of the episodes that actually occur.
According to Harvard Medicine, risk factors for obstructive sleep apnea [12] include:
- Obesity
- Family history of obstructive sleep apnea or snoring
- Certain facial shapes, especially those with a small jaw
- Male gender
- Large neck circumference
- Large tonsils
- Using alcohol at bedtime
- Being post-menopausal
- Hypothyroidism
- Acromegaly
Treating obstructive sleep apnea often requires the use of a CPAP, a device that forces air into your lungs while you sleep. Treatment may also include surgery in some situations. For some people, lifestyle modifications may be enough to improve their obstructive sleep apnea. If you believe you may have obstructive sleep apnea, you should consult with your doctor about potential treatment options.
Restless Leg Syndrome
Restless leg syndrome, also called Willis-Ekbom Disease, is a condition that causes uncomfortable sensations in the legs, creating an almost irresistible urge to move the legs. People with this condition often find that stretching, shaking, or fidgeting their legs helps to alleviate symptoms. Walking may also help to provide relief.
The symptoms of restless leg syndrome are often worse later in the day, especially when resting. Many people with restless leg syndrome find that the symptoms are at their worst when they relax or lie down. This means that lying down and relaxing to go to sleep will cause the symptoms of restless leg syndrome to heighten, making it almost impossible to actually fall asleep.
People who have restless leg syndrome are also likely to have another condition called periodic limb movement disorder. This condition causes limbs to twitch or flex involuntarily while sleeping. While these limb movements do not have the same uncomfortable symptoms that restless leg syndrome does, it can still cause someone to wake up while they are sleeping.
The cause of restless leg syndrome is not fully understood. People with certain medical conditions like Parkinson’s disease, multiple sclerosis, and iron deficiency are more at risk for developing the condition. Pregnancy can also temporarily cause restless leg syndrome. The way in which these conditions increase the risk of restless leg syndrome occurring, however, is not understood.
According to the Sleep Foundation, triggers for restless leg syndrome [13] in those who have it include:
- Sitting
- Resting
- Using alcohol
- Using caffeine
- Using nicotine-containing products
- Using certain medications
Avoiding these triggers when possible, especially the triggers relating to substance use, may help to reduce the incidence of restless leg syndrome.
Restless leg syndrome can be treated with medicines. Most doctors, however, will typically recommend lifestyle changes before trying medical treatments. Exercise and avoiding triggers before bedtime can help to reduce the symptoms of restless leg syndrome. Other measures like massages and hot baths may also be helpful.
Narcolepsy
Narcolepsy is a sleep disorder that doesn’t cause problems getting enough sleep but rather causes sudden sleepiness at times when you should be awake. Someone with narcolepsy may find that they suddenly develop sleepiness or fall asleep unintentionally during the day when they would normally be awake.
The cause of narcolepsy is not fully understood; however, it appears that it is related to low levels of hypocretin, a chemical that promotes wakefulness and regulates REM sleep. There are certain factors that can increase the risk of narcolepsy [14]. These include:
- Autoimmune disorders
- Having a close relative with narcolepsy
- History of brain injury
Most people who experience narcolepsy will only experience it sporadically, making it difficult to identify the underlying problem.
Treatments for narcolepsy can involve medications that stimulate the body and promote wakefulness. Following good sleep hygiene practices and using certain strategies, like taking naps throughout the day, can help to improve symptoms of narcolepsy.
Somnambulism
Somnambulism, more commonly known as sleepwalking, is a condition in which someone walks or performs complex actions while still asleep. Somnambulism is more common in children but can affect people of any age. Someone who is sleepwalking will often be difficult to arouse, will not respond or be incoherent, and will not remember the episode of sleepwalking when they awaken. An episode of sleepwalking may last for up to half an hour.
Somnambulism may cause accidents when someone performs unsafe actions while asleep. It may also lead to tiredness and less restorative sleep. Because someone who sleep walks is not aware of what occurs during an episode, they will not know that they have somnambulism unless someone else observes them performing actions while asleep.
According to the Sleep Foundation, risk factors for somnambulism [15] include:
- Genetics
- Sleep deprivation
- Certain medications
- Using alcohol before sleeping
- Brain injury
- Fever
- Having obstructive sleep apnea
- Having restless leg syndrome
- Stress
Treatment for somnambulism is very dependent upon the individual situation. Often, the focus will be on treating any underlying cause that is making somnambulism occur and instituting safety measures to prevent potential harm while asleep. In some situations, medicine or therapy may be helpful.
Sleep Paralysis
Sleep paralysis [16] is an unusual condition in which someone waking up is unable to move for several seconds or minutes. Episodes of sleep paralysis are often accompanied by hallucinations that are often of a negative nature.
During sleep, especially REM sleep, the body enters a state of paralysis. This helps the person sleeping to avoid acting out dreams while they are sleeping. Sleep paralysis is thought to be caused when someone becomes conscious during sleep, but the paralysis that occurs during sleep is still present.
While sleep paralysis is not well understood, it is not considered to be dangerous and has no significant health effects. An episode of sleep paralysis, however, can be distressing and uncomfortable, making it desirable to avoid.
The risk factors for sleep paralysis are not well understood. There is some evidence that conditions like obstructive sleep apnea can increase the risk of sleep paralysis; however, more research is necessary to fully understand what causes this condition.
The treatment for sleep paralysis primarily involves good sleep hygiene to promote healthy and restorative sleep. Treatments could also include certain types of therapy and medications in some situations.
Sleep Hygiene
One of the best things that someone can do to promote high-quality sleep is to follow good sleep hygiene. The term sleep hygiene [17] refers to following good practices when preparing to sleep that optimize yourself and your environment for sleep.
The core elements of sleep hygiene include:
- A consistent schedule - Going to bed at the same time every night and getting up at the same time every morning helps to regulate your circadian rhythm and your sleep-wake cycle.
- Pre-bed routine - Having a consistent bedtime routine will help provide cues to your body and mind that it is time to sleep, helping your body better recognize that it is time to sleep. A pre-bed routine should be relaxing and help you transition to being ready to sleep.
- Bed comfort - An important element of sleep hygiene is having a comfortable mattress and pillow, as well as having good sheets and blankets. A comfortable environment will make it easier to fall asleep.
- Lighting - Reducing lighting before bed will provide your body with cues that it is time to get ready to sleep. It is especially important to avoid blue lighting in the period right before you go to bed.
- Exercise - Exercising regularly will generally help your body be more ready for sleep and help your sleep to be deeper and more restorative.
- Use your bedroom for sleep - Avoid using your bedroom for activities other than going to sleep and having intercourse. This helps trigger your body and mind to better recognize that it is time to go to sleep when you are in your bedroom.
- Temperature - A temperature of about 65-67 degrees Fahrenheit is ideal for sleeping. Maintaining your bedroom at this temperature can help improve your sleep quality.
- Avoid bedtime eating or certain drinks - Avoiding large meals before bed or using alcohol or caffeine will help you get to sleep better. Some drinks, like a soothing, caffeine-free tea, may help you get to sleep more easily
- Avoid screens before bed - Avoid using electronics with lit screens in the half hour before bed. Screens produce light that triggers your body to stay in the wake part of the sleep-wake cycle. Screens with blue light are especially impactful on your ability to get to sleep.
Red Light Therapy and Sleep
Red light therapy has only recently been applied to improve the quality of sleep but is already an important part of many people’s sleep hygiene. Research indicates that red light wavelengths, which are longer than the shorter wavelengths of white light and blue light, can improve the overall quality of sleep, making you feel more restored and refreshed. Higher quality sleep is also connected with a lower risk of many sleep disorders. Good sleep hygiene is often the first step in managing most sleep disorders, and innovations like red light therapy may help to reduce the problems associated with many sleep-related problems.
Red light therapy offers an ideal resource for those needing help with sleep. Red light is known to not have the same effect on the sleep-wake cycle that other forms of light do. Red light is used in cockpits at night and in submarines because it does not have the same effect on night vision that other wavelengths of light do. Because red light has a low impact on how the brain subconsciously perceives night-related lighting, it offers a potential tool that is unlikely to make you feel more awake while it is dark.
Improvement in Underlying Factors
Many times, an inability to sleep is not exclusively caused by a sleep disorder but also by underlying factors that make sleeping more difficult. Research [18] published in Photobiomodulation, Photomedicine, and Laser Surgery that examined the effects of red light therapy on anxiety found that as treatments improved anxiety, sleep quality improved as well.
Other studies into how red light therapy improves sleep by helping with underlying factors include:
- A study [19] published in Children. This research found that red light therapy could help improve symptoms of autism and also found that, with these improvements, improved sleep quality also occurred.
- Research [20] published in Neuropsychiatric Disease and Treatment. This study indicated that using red light therapy to treat traumatic brain injury (TBI) helped to improve TBI symptoms. Researchers found that, as symptoms of TBI improved, sleep quality also improved.
- A study [21] in the Journal of Neurotrauma. This study used red light therapy to treat chronic, mild traumatic brain injuries. According to this study, “participants reported improved sleep” as well as other improvements of TBI symptoms.
- Research [22] published in BBA Clinical. This review examined existing research and found that the use of red light therapy could improve symptoms caused by stroke, traumatic brain injury, global ischemia, dementia, Alzheimer's disease, Parkinson's disease, depression, anxiety, and post-traumatic stress disorder. One commonly-improved symptom in the literature was sleep disturbances.
Much of the research associated with the use of red light therapy to treat underlying problems causing sleep disturbances has focused on cognitive or mental health-related conditions.
Improved Sleep Quality

The first research indicating that red light therapy improves sleep quality emerged in 2012 and was published in the Journal of Athletic Training. This study [23] followed a group of athletes who received full-body red light therapy compared to a control group. The researchers found that those who received red light therapy had higher levels of melatonin secretion and reported improved sleep quality.
Since this foundational study, many studies have demonstrated that the use of red light can improve sleep quality. Relevant research includes:
- A 2017 study [24] published in Photomedicine and Laser Surgery. This study used a small sample of dementia patients and found that weekly red light therapy for 12 weeks improved sleep. The researchers also noted that this form of therapy was idealistic in that it could be provided at home and avoided many of the complications associated with medications.
- A 2018 study [25] published in Arquivos de Neuro-Psiquiatria. In this study, researchers compared the effects of using botox versus red light therapy in 38 people with migraines. The researchers found that, while both treatments reduced the intensity and severity of migraines, red light therapy was more effective in improving the quality of sleep. This suggests that red light therapy had an effect on sleep beyond just improving the underlying pain that migraine sufferers experienced.
- A 2022 paper [26] published in Frontiers in Neuroscience. In this analysis, researchers examined past research and proposed that there was a difference in how red light therapy affects individuals based on whether they are asleep or awake during therapy. The researchers proposed that red light therapy leads to “more effective in improving the flow of cerebrospinal fluid and clearance of waste from the brain” when delivered while sleeping.
- A 2023 paper [27] published in Neural Regeneration Research. Researchers proposed a mechanism by which red light therapy, delivered while sleeping, may improve sleep quality. This mechanism focused on the glymphatic system of the brain and how red light therapy may affect it.
A 2023 review [28] published in the Journal of Sleep Research. This review, interestingly, analyzed the effects of bright light in general on sleep, not red light specifically. The researchers noted, however, that red light was used as a placebo to replace bright light and was found to have an effect on its own. This research accidentally supported the concept that the use of red light promotes sleep quality.
Decreased Sleep Inertia
Sleep inertia describes a state in which someone is groggy or sluggish after awakening. This can be due to waking up in a deep state of sleep or falling back to sleep after waking, but can also be caused by non-restorative sleep.
Recent research [29] into red light therapy indicates that using red light therapy regularly can decrease sleep inertia. In this study, researchers found increased short-term memory performance when using red light therapy after sleeping. Decreasing sleep inertia can be especially important for those who get a shorter-than-normal amount of sleep, work a night shift schedule, or experience jet lag.
The concept that red light can increase alertness predates most research specifically focusing on red light therapy as a sleep aid. In 2009, research [30] published in BMC Neuroscience noted that exposure to red light at night increased alertness while not affecting the ability to fall asleep. This reinforces that, somewhat counterintuitively, red light therapy that can help make it easier to have high-quality sleep can also help people to feel more alert while they are awake.
Improving Restless Leg Syndrome Symptoms
Restless leg syndrome is a common sleep disorder. Red light therapy research has shown promising results in some early studies as a potential method of improving symptoms of restless leg syndrome. One study [31], published in Physiotherapy: Theory and Practice, found that four weeks of therapy using infrared light improved symptoms of restless leg syndrome. Another well-controlled experiment [32] also found improvements in restless leg syndrome when using infrared wavelengths of light.
Improved Circadian Rhythm
Another important study [33] into how red light therapy affects sleep found that using red light therapy can improve the synchronization of the circadian rhythm and reduce sleepiness during the afternoon. This study applied red light in an office setting and found that the effect it had on workers’ circadian rhythms led to an improvement in energy levels after lunch, a time of day when energy levels often lag. The study also showed improved function of their circadian rhythms.
One study [34] into red light therapy, published in Biology, did demonstrate that using red light therapy in the morning did not improve overall sleep quality. Coupled with other studies, this may suggest that red light therapy’s relationship with the circadian rhythm makes it more effective for sleep when used in the evenings.
In addition to improving the overall circadian rhythm, red light therapy can help to simulate low daytime light. Research [35] published in the Journal of Affective Disorders found that exposure to low daytime lighting has important impacts on mood, sleep, and the circadian rhythm. Red light therapy may help to simulate this lighting and could offer similar benefits to low daytime lighting.
Trying Red Light Therapy For Sleep
Research into how to best use red light therapy to improve sleep quality is still ongoing. Initial research into using it for sleep showed that full-body irradiation provided improved sleep quality and helped to enhance the production of melatonin. Other studies have used red light therapy that is directed into the eyes.
While using red light therapy on your eyes has not been proven to be dangerous, most experts advise caution with this approach due to the fact that LED light therapy devices can be quite bright. Because full body irradiation has been shown to provide subjective improvements in sleep quality, this method of use is generally recommended when using it for sleep promotion.
Because research into red light therapy for sleep is still in its early days, there are no established recommendations for when you should use it. Using it before bed, however, may be beneficial for those who want to improve the quality of their sleep, and it is unlikely that red light exposure prior to bed will make sleeping more difficult.
One study, [36] published in the Journal of Neurotrauma, found that it took at least five treatments for sleep efficiency and cognitive performance to meaningfully improve. This is only one study, and it is not clear what type of red light source and dose were used. This research could, however, indicate that results may take a few days of consistent use to manifest.
Mito Red Light
Not all red light therapy panels are created equal. For red light therapy to be worth the investment, you need a high-quality, independently tested, professional red light therapy device from a reputable company. With over 5 years in business and over 65,000 ecstatic customers, Mito Red Light is a brand you can trust. Our nearly 2,000 reviews speak for themselves. You can also click to review some of our customers' red light therapy before and after examples.
We are confident that our devices are the highest quality and best value at home red light therapy devices available anywhere. We welcome you to review our selection of red light therapy devices or to contact one of our representatives at 1-866-861-6486 to learn more or to help find the right solution for you.
Click to learn more about potential red light therapy benefits.
Find Commercial Mito Red Light Therapy Near Me
To learn more basics about red light therapy, read How Does Red Light Therapy Work?
Related Articles
Green Light Therapy | Explore the Science
Red Light Therapy for Migraines: Does It Help?
Infrared Sauna vs. Red Light Therapy
References:
- NASA. (2022, May 19). NASA research illuminates medical uses of light. https://spinoff.nasa.gov/NASA-Research-Illuminates-Medical-Uses-of-Light
- Tafur, J., & Mills, P. J. (2008). Low-Intensity light therapy: Exploring the role of redox mechanisms. Photomedicine and Laser Surgery, 26(4), 323-328. https://doi.org/10.1089/pho.2007.2184
- National Institute of Neurological Disorders and Stroke. (2023, July 19). Brain basics: Understanding sleep. https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep
- Suni, E., & Vyas, N. (2023, August 8). Stages of sleep. Sleep Foundation. https://www.sleepfoundation.org/stages-of-sleep
- Suni, E., & Singh, A. (2023, August 8). Circadian rhythm. Sleep Foundation. https://www.sleepfoundation.org/circadian-rhythm
- National Center for Complementary and Integrative Health. (2022, July). Melatonin: What you need to know. https://www.nccih.nih.gov/health/melatonin-what-you-need-to-know
- Division of Sleep Medicine at Harvard Medical School. (2021, October 1). Sleep and health. https://sleep.hms.harvard.edu/education-training/public-education/sleep-and-health-education-program/sleep-health-education-86
- Lusardi, P., Zoppi, A., Preti, P., Pesce, R. M., Piazza, E., & Fogari, R. (1999). Effects of insufficient sleep on blood pressure in hypertensive patients: a 24-h study. American Journal of Hypertension, 12(1 Pt 1), 63-68. https://doi.org/10.1016/s0895-7061(98)00200-3
- Chaput, J.-P., Després, J.-P., Bouchard, C., & Tremblay, A. (2008). The association between sleep duration and weight gain in adults: A 6-year prospective study from the Quebec Family Study. Sleep, 31(4), 517-523. https://doi.org/10.1093/sleep/31.4.517
- Centers for Disease Control and Prevention. (2022, July 28). Sleep for a good cause. https://www.cdc.gov/diabetes/
- Suni, E., & Rehman, A. (2023, August 8). Insomnia: What it is, how it affects you, and how to help you get back your restful nights. Sleep Foundation. https://www.sleepfoundation.org/insomnia
- LeWine, H. E. (2023, June 24). Sleep apnea. Harvard Health Publishing. https://www.health.harvard.edu/a_to_z/sleep-apnea-a-to-z
- Pacheco, D., & Wright, H. (2023, July 11). Restless Legs Syndrome (RLS): What it is, its causes and symptoms, and how it can be addressed to improve sleep. Sleep Foundation. https://www.sleepfoundation.org/restless-legs-syndrome
- National Institute of Neurological Disorders and Stroke. (n.d.). Narcolepsy. https://www.ninds.nih.gov/health-information/disorders/narcolepsy
- Suni, E., & Vyas, N. (2023, August 14). Sleepwalking: What is Somnambulism? Sleep Foundation. https://www.sleepfoundation.org/parasomnias/sleepwalking
- Farooq, M., & Anjum, F. (2023). Sleep Paralysis. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK562322/
- Centers for Disease Control and Prevention. (2022, September 13). Tips for better sleep. https://www.cdc.gov/sleep/about/index.html
- Maiello, M., Losiewicz, O. M., Bui, E., Spera, V., Hamblin, M. R., Marques, L., & Cassano, P. (2019). Transcranial Photobiomodulation with Near-Infrared Light for Generalized Anxiety Disorder: A Pilot Study. Photomedicine and Laser Surgery, 37(10), 644-650. https://doi.org/10.1089/photob.2019.4677
- Pallanti, S., Di Ponzio, M., Grassi, E., Vannini, G., & Cauli, G. (2022). Transcranial Photobiomodulation for the Treatment of Children with Autism Spectrum Disorder (ASD): A Retrospective Study. Children, 9(5), 755. https://doi.org/10.3390/children9050755
- Morries, L. D., Cassano, P., & Henderson, T. A. (2015). Treatments for traumatic brain injury with emphasis on transcranial near-infrared laser phototherapy. Neuropsychiatric Disease and Treatment, 11, 2159-2175. https://doi.org/10.2147/NDT.S65809
- Naeser, M. A., Zafonte, R., Krengel, M. H., Martin, P. I., Frazier, J., Hamblin, M. R., ... & Baker, E. H. (2014). Significant improvements in cognitive performance post-transcranial, red/near-infrared light-emitting diode treatments in chronic, mild traumatic brain injury: open-protocol study. Journal of Neurotrauma, 31(11), 1008-17. https://doi.org/10.1089/neu.2013.3244
- Hamblin, M. R. (2016). Shining light on the head: Photobiomodulation for brain disorders. BBA Clinical, 6, 113-124. https://doi.org/10.1016/j.bbacli.2016.09.002
- Zhao, J., Tian, Y., Nie, J., Xu, J., & Liu, D. (2012). Red Light and the Sleep Quality and Endurance Performance of Chinese Female Basketball Players. Journal of Athletic Training, 47(6), 673-678. https://doi.org/10.4085/1062-6050-47.6.08
- Saltmarche, A. E., Naeser, M. A., Ho, K. F., Hamblin, M. R., & Lim, L. (2017). Significant Improvement in Cognition in Mild to Moderately Severe Dementia Cases Treated with Transcranial Plus Intranasal Photobiomodulation: Case Series Report. Photomedicine and Laser Surgery, 35(8), 432-441. https://doi.org/10.1089/pho.2016.4227
- Loeb, L. M., Amorim, R. P., Mazzacoratti, M. G. N., Scorza, F. A., & Peres, M. F. P. (2018). Botulinum toxin A (BT-A) versus low-level laser therapy (LLLT) in chronic migraine treatment: a comparison. Arquivos de Neuro-Psiquiatria, 76(10), 663-667. https://doi.org/10.1590/0004-282X20180109
- Moro, C., Valverde, A., Dole, M., Kam, J. H., Hamilton, C., Liebert, A., ... & Mitrofanis, J. (2022). The effect of photobiomodulation on the brain during wakefulness and sleep. Frontiers in Neuroscience, 16. https://doi.org/10.3389/fnins.2022.942536
- Valverde, A., Hamilton, C., Moro, C., Billeres, M., Magistretti, P., & Mitrofanis, J. (2023). Lights at night: does photobiomodulation improve sleep? Neural Regeneration Research, 18(3), 474-477. https://doi.org/10.4103/1673-5374.350191
- Chambe, J., Reynaud, E., Maruani, J., Fraih, E., Geoffroy, P. A., & Bourgin, P. (2023). Light therapy in insomnia disorder: A systematic review and meta-analysis. Journal of Sleep Research. https://doi.org/10.1111/jsr.13895
- Figueiro, M. G., Sahin, L., Roohan, C., Kalsher, M., Plitnick, B., & Rea, M. S. (2019). Effects of red light on sleep inertia. Nature and Science of Sleep, 11, 45-57. https://doi.org/10.2147/NSS.S195563
- Figueiro, M. G., Bierman, A., Plitnick, B., & Rea, M. S. (2009). Preliminary evidence that both blue and red light can induce alertness at night. BMC Neuroscience, 10, 105. https://doi.org/10.1186/1471-2202-10-105
- Mitchell, U. H., Johnson, A. W., & Myrer, B. (2011). Comparison of two infrared devices in their effectiveness in reducing symptoms associated with RLS. Physiotherapy Theory and Practice, 27(5), 352-9. https://doi.org/10.3109/09593985.2010.502210
- Mohammadi, M. M., Vaisi Raygani, A. A., Ghobadi, A., Samadzadeh, S., & Salari, N. (2018). Effect of Near-Infrared Light Therapy Based on Acupoints on the Severity of Restless Legs Syndrome in Patients Undergoing Hemodialysis: A Single-Blind, Randomized Controlled Trial. Clinical Medicine Research, 16(1-2), 1-8. https://doi.org/10.3121/cmr.2018.1389
- Figueiro, M. G., Steverson, B., Heerwagen, J., Yucel, R., Roohan, C., Sahin, L., Kampschroer, K., & Rea, M. S. (2019). Light, entrainment and alertness: A case study in offices. Lighting Research and Technology, 52(6). https://doi.org/10.1177/1477153519885157
- Giménez, M. C., Luxwolda, M., Van Stipriaan, E. G., Bollen, P. P., Hoekman, R. L., Koopmans, M. A., ... & Gordijn, M. C. M. (2022). Effects of Near-Infrared Light on Well-Being and Health in Human Subjects with Mild Sleep-Related Complaints: A Double-Blind, Randomized, Placebo-Controlled Study. Biology, 12(1), 60. https://doi.org/10.3390/biology12010060
- Burns, A. C., Saxena, R., Vetter, C., Phillips, A. J. K., Lane, J. M., & Cain, S. W. (2021). Time spent in outdoor light is associated with mood, sleep, and circadian rhythm-related outcomes: A cross-sectional and longitudinal study in over 400,000 UK Biobank participants. Journal of Affective Disorders, 295, 347-352. https://doi.org/10.1016/j.jad.2021.08.056
- Zhao, X., Du, W., Jiang, J., & Han, Y. (2022). Brain Photobiomodulation Improves Sleep Quality in Subjective Cognitive Decline: A Randomized, Sham-Controlled Study. Journal of Alzheimer's Disease, 87(4), 1581-1589. https://doi.org/10.3233/JAD-215715