DISCLAIMER: Mito Red Light devices are Class II wellness devices aimed at affecting the body through topical heating and supporting cellular function. The information provided in this article and on this site is for educational purposes only and is not intended to imply effectiveness of Mito Red Light devices for any specific application. The information provided in this article and on this site is not intended to diagnose, treat, cure, or prevent any disease, is not a substitute for consultation with a licensed medical provider and should not be construed as medical advice. Click here to read our article on potential contraindications of red light therapy..
Authored by Benjamin Caleb Williams.
Article at a Glance:
- Millions of people suffer from migraines, which significantly impact their quality of life.
- Traditional migraine treatments often have side effects and limitations, prompting interest in natural alternatives.
- Narrowband green light therapy has emerged as a potential, non-invasive solution for reducing migraine pain and frequency.
- Migraines involve complex neurological factors, and symptoms can range from intense head pain to sensory disturbances.
- Recognizing common migraine triggers is a vital part of managing them effectively.
- Holistic migraine management strategies can complement traditional and alternative treatments.
- The MitoGREEN™ combines narrowband green light, into a portable red light therapy device for a versatile, comprehensive, multi-layered approach to managing migraines and promoting overall wellness.
Millions of people worldwide suffer from migraines [1]. These painful headaches not only cause severe physical pain but also cause significant disruptions to everyday life. As anyone who has experienced a migraine can attest, the throbbing headaches can make even the simplest tasks feel insurmountable.
For those who struggle with migraines regularly, the quest for effective, long-term relief is an ongoing challenge. While traditional treatments can sometimes offer help, they often come with limitations and unwanted side effects. As a result, a growing number of people are exploring holistic and natural solutions, hoping to manage their migraines in a safer and more sustainable way.
One recent and promising avenue is narrowband green light therapy. In recent years, researchers and wellness enthusiasts alike have turned their attention to the therapeutic potential of specific light wavelengths. Early findings suggest that green light therapy specifically could offer meaningful relief to migraine sufferers by reducing pain intensity and frequency.
In this article, we’ll delve into the intricacies of migraines, review traditional treatment approaches, and explore how narrowband green light combined with red light therapy could be a game changer for those seeking to reclaim their quality of life.
Understanding Migraines
Migraines are more than just bad headaches; they are a complex neurological condition that can present in various forms and severity. Surprisingly, the exact causes of migraines remain elusive, and researchers still do not fully understand what causes them.
While migraines are still being researched, it is clear that they involve abnormal brain activity that affects nerve pathways, brain chemicals, and blood flow. These disturbances can result in the intense, pulsating pain many sufferers experience, typically on one side of the head, often accompanied by other incapacitating symptoms.
For those living with migraines, it’s not just the pain but the unpredictability that takes a significant toll [2] on their lives. Migraines can last anywhere from a few hours to several days, and they can occur with or without warning. This uncertainty adds to the stress and anxiety that many sufferers feel, as they constantly worry about when the next attack might strike. To manage migraines effectively, it’s crucial to understand the common symptoms and potential triggers.
Symptoms
Migraine symptoms vary from person to person, but some are common and often serve as telltale signs of an impending or active migraine attack. Understanding these symptoms [3] can help sufferers prepare and manage their condition more effectively.
- Severe, throbbing, or pulsing pain, usually affecting one side of the head.
- Sensitivity to light, sound, and sometimes smell.
- Nausea and vomiting.
- Auras (visual disturbances, such as flashing lights or blind spots, that can precede or accompany a migraine).
- Tingling or numbness in the face or extremities.
- Dizziness or a feeling of lightheadedness.
- Difficulty speaking or concentrating.
- Fatigue and general malaise following the migraine.
These symptoms not only relate to the intensity of migraines but also underscore how they affect multiple bodily functions. Understanding the wide range of symptoms can make it easier to understand exactly how migraines can affect you and help as you seek appropriate interventions and relief.
Triggers
The exact triggers for migraines [4] are often highly individual, making it difficult to identify a one-size-fits-all approach to prevention. However, many sufferers report several common triggers that may apply to your situation. By recognizing and monitoring these triggers, individuals can take proactive steps to reduce the frequency and severity of their attacks.
Some of the most prevalent triggers include:
- Hormonal changes - Hormonal changes, particularly in women, such as fluctuations during the menstrual cycle, pregnancy, or menopause.
- Food and drink triggers - Caffeine, alcohol (especially red wine), aged cheeses, and foods with additives like MSG can all be common migraine triggers.
- Stress - Any kind of stress, whether acute or chronic, can increase the likelihood of migraines.
- Sleep disturbances - Both lack of sleep and oversleeping can be triggers.
- Sensory stimuli - Bright lights, loud noises, or strong smells can both trigger migraines and make them worse.
- Changes in weather - Barometric pressure changes, particularly decreased air pressure that accompanies bad weather, can trigger migraines.
- Medication overuse - This is especially true with pain relievers that can create rebound headaches.
These triggers show how diverse the factors are that can set off a migraine attack. Identifying triggers often requires detailed tracking and attentiveness to how your body is responding to what is happening around you. For trigger recognition to help, you may need to be willing to adapt lifestyle choices, which can be challenging. However, even partial control over triggers can make a significant difference.
Despite efforts to avoid triggers, migraines may still strike, making it important to understand the impact of this condition on daily life is essential.
Impact on Life
The toll that migraines take on an individual’s well-being can extend far beyond the physical pain they cause, meaningfully affecting their quality of life [5] in several ways. From a professional perspective, migraines are a leading cause of missed workdays and reduced productivity. The economic burden of absenteeism and lost performance can be considerable, not just for sufferers but also for employers and healthcare systems.
On a personal level, migraines can disrupt family dynamics, limit social engagements, and reduce an individual’s overall quality of life. The cumulative effect of this chronic condition often leads to feelings of isolation, frustration, and even depression, as sufferers struggle to balance daily responsibilities with the unpredictability of their health.
Traditional Approaches to Migraine Relief: Limitations and Side Effects
For many individuals dealing with migraines, traditional treatments [6] are often the first line of defense. These treatments are generally designed to either prevent migraines from occurring or to alleviate symptoms once an attack has started. While they can be effective, many conventional approaches can come with limitations and notable side effects that leave sufferers seeking alternative or complementary options.
Common Treatment Options
The medical community has developed various pharmaceutical [7] and non-pharmaceutical options to help manage migraines. Some of these focus on acute relief, while others aim to minimize the frequency and intensity of attacks. Here’s an overview of some of the most common migraine treatments:
- Over-the-counter pain relievers. Medications like aspirin, ibuprofen, or acetaminophen are often used for mild to moderate migraine attacks.
- Prescription medications. Drugs such as triptans, ergotamines, and anti-nausea medications can be prescribed for more severe migraine symptoms.
- Preventive medications. Options like beta-blockers, antidepressants, and anti-seizure drugs help reduce the frequency of migraines for individuals who suffer chronically.
- CGRP inhibitors. This newer class of drugs has shown promise in preventing migraines by blocking pathways associated with migraine attacks.
- Botox injections. Approved for chronic migraine prevention, botox can help reduce the number of headache days experienced each month.
- Lifestyle modifications. Strategies like regular exercise, dietary adjustments, and ensuring adequate sleep can be crucial components of a comprehensive migraine management plan.
While these treatments can provide relief for many, they also come with challenges, costs, and side effects that can make them undesirable as a long-term solution.
Limitations of Traditional Treatments
Despite the availability of numerous pharmaceutical options, traditional migraine treatments often come with limitations that make them less appealing in the long term. One major issue is the variability of effectiveness. A medication that works well for one person may do little for another. This inconsistency can be incredibly frustrating for sufferers, leading to a long and often exhausting process of trial and error to find a treatment that works.
Many migraine medications have side effects that can be almost as debilitating as the migraines themselves. For example, over-the-counter pain relievers, if overused, can lead to rebound headaches, while prescription drugs like triptans may cause dizziness, fatigue, or tightness in the chest. Preventive medications can also be problematic; beta-blockers can lower blood pressure excessively, and antidepressants may cause mood swings or weight gain. These side effects sometimes force individuals to discontinue treatment, leaving them with limited options for relief.
The emergence of medication overuse headaches is another significant concern. People who rely heavily on pain medications may find themselves caught in a cycle where their frequent use of these drugs actually contributes to more headaches, exacerbating the problem they’re trying to solve.
Many migraine treatment options are also expensive over a long-term basis. For example, botox injections can cost thousands of dollars with each treatment. Some specialty migraine medications can cost $100 per pill or more. With costs like these, more sustainable options are often quite appealing.
Why People Are Exploring Alternative Options
The limitations and side effects of traditional migraine treatments have driven many people to explore alternative and holistic options. For those who prioritize natural approaches to health and wellness, the allure of treatments that align with the body’s natural healing processes is strong.
Another driving factor is the desire to minimize pharmaceutical dependence, especially for chronic conditions. As scientific research expands our understanding of migraines and their triggers, new light-based therapies, such as narrowband green light, are becoming increasingly appealing. People are eager to find ways to manage their migraines effectively without compromising their overall well-being.
27 Tips for Holistic Migraine Management
Holistic migraine management [8] goes beyond symptom relief; it focuses on overall well-being and minimizing migraine frequency through lifestyle choices, natural remedies, and self-care strategies. Combining these approaches with treatments like green light therapy may yield even more significant benefits. By making small but impactful changes to daily routines, individuals can create an environment less conducive to migraine triggers.
A balanced approach to wellness includes everything from diet and exercise to mindfulness and stress management. It's essential to recognize that migraines are highly individualized, meaning that a strategy that works for one person may not be as effective for another. Therefore, having a diverse toolkit of techniques can empower individuals to find what works best for them.
Here are several holistic tips [9] to help manage migraines and promote a healthier lifestyle overall:
- Stay hydrated - Drink plenty of water throughout the day to prevent dehydration, a common migraine trigger.
- Maintain a consistent sleep schedule - Aim for the same bedtime and wake time daily, even on weekends.
- Incorporate regular exercise - Low-impact activities like walking, swimming, or yoga can reduce stress and promote overall wellness.
- Limit processed foods - Focus on a diet rich in whole foods like vegetables, fruits, and lean proteins.
- Keep a migraine diary - Tracking symptoms and triggers can help identify patterns and manage attacks more effectively.
- Practice mindfulness meditation - Techniques such as deep breathing can help manage stress, a common trigger.
- Try acupuncture - This traditional Chinese practice may help reduce the frequency of migraines in some individuals.
- Invest in blackout curtains - Reducing exposure to light, especially during an attack, can help ease symptoms.
- Consider essential oils - Lavender or peppermint oil, when applied to the temples or inhaled, can have a calming effect for some people.
- Incorporate magnesium-rich foods - Magnesium deficiencies are linked to migraines, so eat more foods with magnesium, like leafy greens and nuts.
- Reduce screen time - Take breaks from devices and use blue light filters to minimize strain on the eyes.
- Explore biofeedback therapy - This technique helps control physiological functions like muscle tension and heart rate.
- Maintain good posture - Slouching can lead to tension headaches, which may trigger a migraine.
- Limit alcohol and caffeine - These substances can be major triggers for some individuals.
- Stay away from strong odors - Perfumes, cleaning products, and certain chemicals can act as triggers.
- Schedule regular massages - Massage therapy can relieve tension and improve blood circulation.
- Use cold or warm compresses - Experiment with both to see which helps relieve your pain more effectively.
- Create a calming environment - Dim the lights, play soft music, and reduce noise to help alleviate migraine discomfort.
- Explore chiropractic care - Spinal adjustments may help reduce headache frequency or intensity in some individuals.
- Stay organized and minimize clutter - A tidy space can help reduce stress and promote a sense of calm.
- Avoid skipping meals - Consistent nutrition helps keep your body in balance.
- Engage in creative activities - Painting, writing, or other hobbies can act as stress relievers.
- Seek support from others - Joining a migraine support group can offer emotional relief and practical tips.
- Use green light therapy regularly - Incorporate sessions into your routine to manage pain and photophobia.
- Practice gratitude - Daily reflection on positive aspects of life can improve mental well-being and reduce stress.
Implementing these holistic practices can have a profound impact on migraine management. Finding what combination of strategies works best may take some time, but the potential improvements to your well-being are well worth the effort.
Narrowband Green Light (520nm): A Promising Solution for Migraine Relief
Amidst the growing exploration of alternative therapies for migraines, narrowband green light [10] has emerged as an exciting and promising solution. Unlike traditional methods that often rely on medication and its associated side effects, green light therapy presents a non-invasive approach that uses specific wavelengths of light to bring relief.
This approach is backed by both early research and anecdotal evidence indicating that exposure to narrowband green light could reduce the intensity and frequency of migraine attacks. As science delves deeper into the mechanisms behind light-based therapies, more people are considering it as a valuable addition to their migraine management toolkit.
Overview of Green Light
Green light therapy is a form of phototherapy that utilizes a narrow band of the visible light spectrum, specifically around the 520nm wavelength. This approach is thought to work by targeting specific pathways in the brain and eyes that are associated with light sensitivity and pain modulation. Narrowband green light therapy focuses on delivering just the right wavelength to maximize these potential benefits while minimizing the adverse effects commonly linked to light exposure.
What Effect Can Green Light Have?
Most wavelengths of light, especially in the blue spectrum, have been shown to increase the intensity of migraines. Green light, however, demonstrates improvement in migraine symptoms. While the mechanisms are not fully understood, this offers a new means of potentially treating migraine.
The effects of narrowband green light therapy are believed to extend beyond mere symptom relief. Researchers have proposed that this wavelength can influence brain activity, particularly in areas involved in pain processing and sensory modulation. While early research has shown that green light therapy holds promise for migraine sufferers, this research is in its infancy, and exactly how it affects the brain will still require more study.
By potentially calming overactive pain pathways and reducing the photophobia that exacerbates migraine discomfort, green light therapy holds promise as a holistic approach to managing migraines. The non-invasive nature of this therapy offers an attractive option for those wary of medication side effects or who wish to supplement their existing treatment plan.
What Does the Research Say About Green Light Therapy and Migraines?
Research into green light therapy for migraines is very new. This specific area of research first gained awareness in 2016, with a ground-breaking study Dr. Rami Burstein's team at Harvard - published in Brain. This study, titled “Migraine photophobia originating in cone-driven retinal pathways,” [11], delved into the effects of various light wavelengths on photophobia and migraine pain. Researchers found that green light had a significantly lesser impact on exacerbating headache pain compared to white, blue, amber, and red lights. They also found that some forms of green light not only didn’t worsen headaches in some patients but, actually caused a meaningful reduction in pain intensity when people were exposed to low-intensity green light.
This study both examined brain activity in human subjects, along with more invasive thalamic neuron recordings in rats. The research revealed that green light activates specific retinal pathways less intensely than other wavelengths of light. This leads to reduced activation of pain-processing neurons in the thalamus. These findings support the potential of green light therapy as a non-pharmacological approach to reducing migraine severity and alleviating photophobia by modulating pain pathways from the retina to the thalamus.

The University of Arizona's studies [10] corroborate many of Burstein's initial findings, adding further weight to the body of evidence supporting green light therapy for migraines. Their clinical trials report not only a decrease in headache frequency and intensity but also huge improvements in quality of life metrics among participants.
These studies built on previous research that had laid the groundwork of demonstrating that green light has healing properties. A study [12] published in Wound Repair and Regeneration used animal models to demonstrate that green LED light significantly accelerated wound healing in mice.
Parallel cell studies in this study indicated that human skin cells exposed to green LED light exhibited increased production of critical healing molecules. The research concludes that green LED light can enhance the body's natural healing mechanisms, providing a non-invasive approach to boosting cellular growth and migration. This study may help direct a better future understanding of how green light therapy impacts migraine symptoms.
Using Green Light Therapy Effectively
Green light therapy is gaining traction as a non-invasive, drug-free option for migraine relief. However, like any wellness practice, it’s essential to understand how to use it safely and effectively to maximize its benefits. The key to successful green light therapy is consistency and proper application, as well as an awareness of any specific safety considerations unique to your health situation. By being mindful of how and when to use the therapy, you can integrate it seamlessly into your daily or weekly routine, giving yourself a natural tool in the ongoing battle against migraines.
How to Get Started
Beginning green light therapy for migraine relief doesn’t have to be complicated. The first step is to invest in a reliable device that emits a narrowband wavelength of approximately 520nm, specifically designed for therapeutic purposes. At Mito Red Light, we combine this wavelength with infrared wavelengths to combine the benefits of green light for migraines with the anti-inflammatory effects of red light.
There is not necessarily a “right” way to use green light for headaches, as the research is not advanced enough to be able to make a definitive recommendation. A common way to use green light for headaches is to start with short, 10-15 minute sessions in a dimly lit or darkened room to enhance the light’s soothing effect on your brain and eyes. Over time, you may find it helpful to gradually increase the session duration depending on how you respond to the treatment. For best results, aim to use the therapy consistently, such as every day or every other day, even on days when you don’t experience migraine symptoms. Regular exposure can be key in reducing the frequency and severity of future attacks.
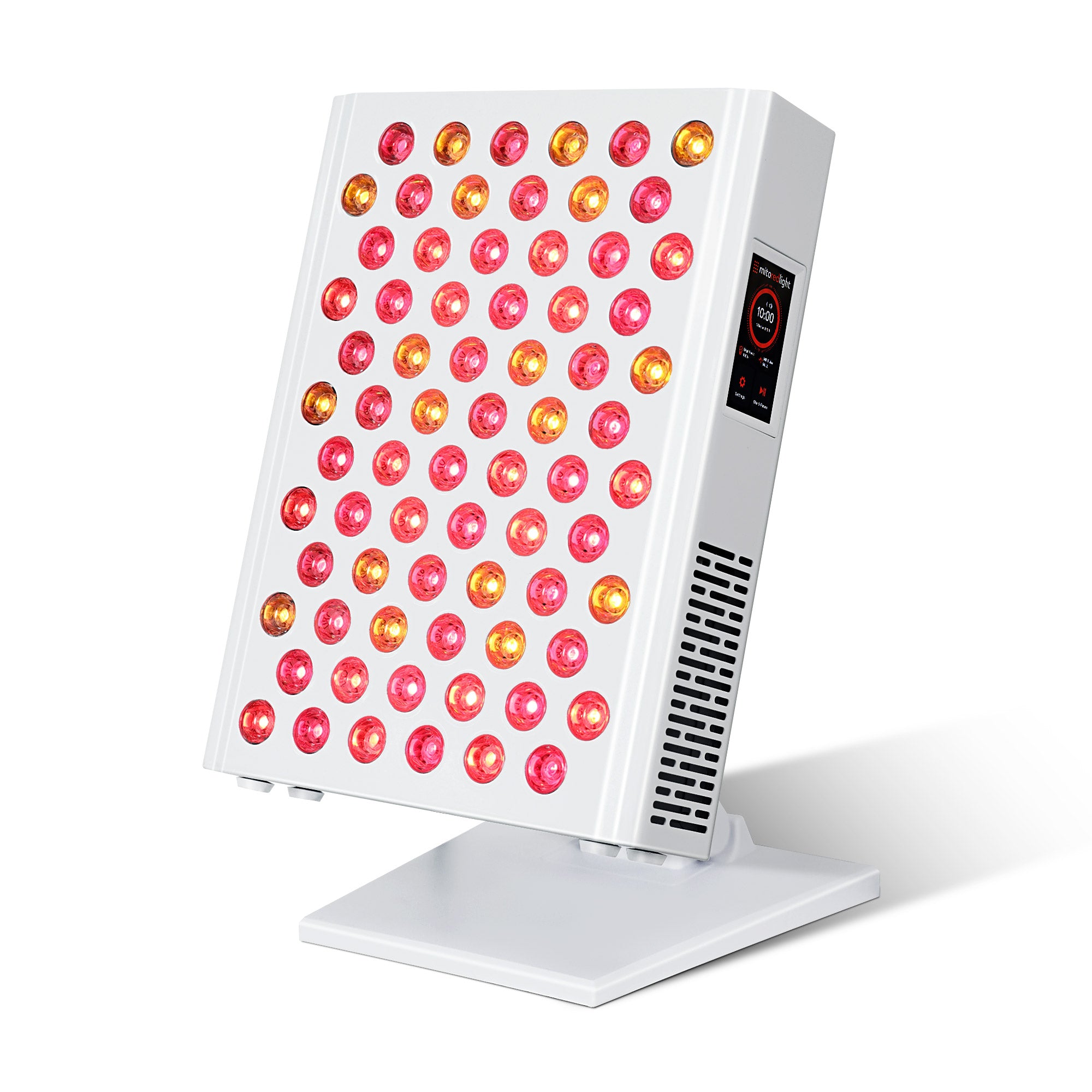
Discover the Benefits of the MitoGREEN™
For those serious about exploring advanced solutions for migraine relief, the MitoGREEN™ is a product designed to revolutionize the way we think about light therapy for headaches. Combining narrowband green light at 520nm and red and near-infrared (NIR) light into one device, the MitoGREEN is a unique. comprehensive, multi-faceted and versatile light therapy device.

While most green light devices on the market only offer the soothing effects of green light, MitoGREEN sets itself apart by integrating both red and NIR light modes. This combination not only addresses immediate migraine symptoms but also leverages the anti-inflammatory and cellular healing benefits associated with red and NIR wavelengths.

Why Combine Red, NIR and Green Light Into One Device?
The MitoGREEN™ is designed with versatility in mind. The MitoGREEN™ has three distinct modes
- Mode 1 - 520nm Green Light only: As needed up to 30 minutes, through closed eyes.
- Mode 2 - Green plus Near Infrared (invisible): As needed up to 10 minutes, through closed eyes.
- Mode 3 - Red + Near Infrared: 10 minutes (max 20 minutes) - eye protection recommended when using into the face.
Why is there a mode that combines green and near infrared?
The studies referenced above using green light and showing benefits for migraines, use ONLY narrowband green light at 520nm (Mode 1).
However, because near infrared is invisible and may have anti-inflammatory properties as well as supporting cellular function, it is theoretically possible the green + NIR helps some people better than green alone. Hence, we have included this combination (Mode 2), so that users have the option to try it.
Also we believe that providing a device that is also a fully functional portable red and NIR therapy light opens up additional healing possibilities. Red and NIR light have long been studied for their roles in promoting cellular repair, reducing inflammation, and boosting circulation. These effects are crucial because inflammation and poor blood flow are often implicated in the cycle of migraine pain.
By incorporating red and NIR light, MitoGREEN aims to offer a holistic experience that addresses not just acute issues but the underlying factors that may contribute to migraine frequency. For instance, red light can penetrate deeper layers of the skin and tissues, helping to calm inflamed nerves and enhance cellular function. NIR light, known for its deep tissue penetration, can promote mitochondrial health, which is essential for energy production and cell recovery. This dual approach means that MitoGREEN may deliver both immediate and long-lasting benefits.
The MitoGREEN
The MitoGREEN is the first of its kind, combining green, red and NIR into one device. It stands out in its uniqueness as well as its dedication to quality and precision. The narrowband 520nm green light sits under frosted lenses with wider beam angle to ensure a more modest intensity. Conversely, the red and NIR dual chip LEDs sit under more narrow focusing lenses, ensuring a fully functional, powerful portable red light therapy device.
While green light can be used to address the immediate headache, red and NIR may offer an additional longer-term anti-inflammatory effect. Together, these modes have the potential to create a multi-layered approach to managing migraines and promoting overall wellness. For anyone dedicated to a lifestyle centered on natural and holistic health, the MitoGREEN™ represents an innovative approach.
Conclusion
While traditional treatments offer options for managing debilitating migraines, they often come with limitations that leave sufferers searching for complementary or alternative solutions. Narrowband green light therapy is one of the newest migraine therapy options, offering a non-invasive and gentle approach.
As research continues to uncover the benefits of light therapy, innovations like MitoGREEN™ are leading the way in integrating this knowledge into practical, user-friendly devices.
Mito Red Light
At Mito Red Light, we provide phototherapy products designed to help you optimize your health in a variety of ways. We welcome you to review our red light therapy products or to contact one of our expert representatives at 1-866-861-6486(MITO) to learn more.
Related Articles:
- EVERYTHING you need to know about Red Light Therapy and Hair Growth
- Red Light Therapy Benefits Overview
- 8 Surprising Benefits of Blue Light Therapy for Acne-Prone Skin
References:
- National Institute of Neurological Disorders and Stroke. (2024, August 1). Migraine. U.S. Department of Health and Human Services. https://www.ninds.nih.gov/health-information/disorders/migraine
- Davies, P. T. G., Lane, R. J. M., Astbury, T., Fontebasso, M., Murphy, J., & Matharu, M. (2018). The long and winding road: The journey taken by headache sufferers in search of help. Primary Health Care Research & Development, 20, e32. https://doi.org/10.1017/S1463423618000324
- Pescador Ruschel, M. A., & De Jesus, O. (2024). Migraine headache. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560787/
- Kesserwani, H. (2021). Migraine triggers: An overview of the pharmacology, biochemistry, atmospherics, and their effects on neural networks. Cureus, 13(4), e14243. https://doi.org/10.7759/cureus.14243
- Al Ghadeer, H. A., AlSalman, S. A., Albaqshi, F. M., Alsuliman, S. R., Alsowailem, F. A., Albusror, H. A., AlAbdi, Z. I., Alwabari, E. M., Alturaifi, Z. A., & AlHajji, A. M. (2021). Quality of life and disability among migraine patients: A single-center study in AlAhsa, Saudi Arabia. Cureus, 13(11), e19210. https://doi.org/10.7759/cureus.19210
- Jenkins, B. (2020). Migraine management. Australian Prescriber, 43(5), 148–151. https://doi.org/10.18773/austprescr.2020.047
- Pellesi, L., Do, T. P., & Hougaard, A. (2024). Pharmacological management of migraine: Current strategies and future directions. Expert Opinion on Pharmacotherapy, 25(6), 673–683. https://doi.org/10.1080/14656566.2024.2349791
- Befus, D. R., Hull, S., Strand de Oliveira, J., Sanders Schmidler, G., Weinberger, M., & Coeytaux, R. R. (2019). Nonpharmacological self-management of migraine across social locations: An equity-oriented, qualitative analysis. Global Advances in Health and Medicine, 8, 2164956119858034. https://doi.org/10.1177/2164956119858034
- Institute for Quality and Efficiency in Health Care (IQWiG). (2022, August 4). Migraine: Learn more – Migraine prevention in adults. In InformedHealth.org. https://www.ncbi.nlm.nih.gov/books/NBK328460/
- Martin, L. F., Patwardhan, A. M., Jain, S. V., Salloum, M. M., Freeman, J., Khanna, R., Gannala, P., Goel, V., Jones-MacFarland, F. N., Killgore, W. D. S., Porreca, F., & Ibrahim, M. M. (2021). Evaluation of green light exposure on headache frequency and quality of life in migraine patients: A preliminary one-way cross-over clinical trial. Cephalalgia, 41(2), 135–147. https://doi.org/10.1177/0333102420956711
- Noseda, R., Bernstein, C. A., Nir, R.-R., Lee, A. J., Fulton, A. B., Bertisch, S. M., Hovaguimian, A., Cestari, D. M., Saavedra-Walker, R., Borsook, D., Doran, B. L., Buettner, C., & Burstein, R. (2016). Migraine photophobia originating in cone-driven retinal pathways. Brain, 139(7), 1971–1986. https://doi.org/10.1093/brain/aww119
- Fushimi, T., Inui, S., Nakajima, T., Ogasawara, M., Hosokawa, K., & Itami, S. (2012). Green light emitting diodes accelerate wound healing: Characterization of the effect and its molecular basis in vitro and in vivo. Wound Repair and Regeneration, 20(2), 226–235. https://doi.org/10.1111/j.1524-475X.2012.00771.x